 I remember a time back in early grade school when the teachers would test observation skills by giving the class pictures to compare. “One of these things is not like the other one” is the first verse to the old Sesame Street song used to teach children similar skills. In medical litigation, similar skills are often employed to ferret out contradictions in medical charting.
I remember a time back in early grade school when the teachers would test observation skills by giving the class pictures to compare. “One of these things is not like the other one” is the first verse to the old Sesame Street song used to teach children similar skills. In medical litigation, similar skills are often employed to ferret out contradictions in medical charting.
Sometimes a comparison between the electronic medical record and the IV pump data will show contradictions that cannot be explained by witness testimony. Sometimes contradictions are between the nursing notes and those notes made by the physician. Sadly, and most disturbingly, is when the contradictions found are those between the electronic medical record and the actual audit trail.

There is a scene in the Twentieth Century Fox blockbuster, Star Wars: The Phantom Menace, where the young, barely 40-inch-tall Anakin Skywalker casts a large misshapen shadow on a wall that vaguely resembles his much later self, Darth Vader. In the movie, this device is used to give a foreshadowing of the future of the young man and the dark path he would take in life. Again, the actual figure and the shadow are contradictions to one another symbolizing things out of place. The trained professionals at ADROITSM look for such out of place or misshapen items when it is suspected that changes to the medical record or even the audit trail have been made to cover up errors. This level of forensic nurse examination is one of the hallmark items that sets ADROITSM apart from the garden variety legal nurse consultants that seem to be ubiquitous on the internet.
To illustrate this point, read the following case study drawn from an actual case. A review of this case will illustrate why ADROITSM should be a key part of your litigation strategy.
Case Study 1: Jane
Jane presented to the hospital on September 29, 2015 for her thrombectomy procedure as scheduled. The records support Jane arrived at or around 11:20 AM. Jane was registered and placed in the Surgical Holding Area at or around 12:40 PM.
Perioperative Nurse Alpha documented at 13:46 (1:46 PM), she gave Jane Valium 10 mg by mouth, started her peripheral IV with IV fluids in preparation for the thrombectomy procedure.
Jane was moved to the Sedation/Procedure room #20, at 15:17 (3:17 P 1M). Sedation Nurse Beta verified the following vital signs, 133/96-108-92% room air.
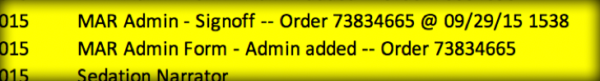
According to documentation by Sedation Nurse Beta, she administered Lopressor 5mg IV-push at 15:38 (3:38 PM) and 0.5 mg of Versed IV-push at 15:38 (3:39 PM) as ordered by Vascular Surgeon, Dr. Charlie. Sedation Nurse Beta validated the following vital signs, 137/99-99-100% on 2L, (excluding blood pressure vitals are taken by the monitor every minute) NOTE: Only those vitals that are validated appear in the medical record. Sedation Nurse Beta documents a second dose of Versed 0.5 mg as given at 15:45 (3:45 PM).
Documentation reflects that at 15:46 (3:46 PM), a one-click med was entered for Lopressor 5mg IV.
One-click meds, enter an order, acknowledge the order and document the med as given, all with one click in these pre-set narrators, like a sedation narrator.

According to the audit trail provided, the documentation supported that Sedation Nurse Beta altered the time given to 15:38 (3:38 PM).This is confirmed in the Audit Trail.
According to Sedation Nurse Beta, she administered Fentanyl 25 mcg IV-push at 15:48 (3:48 PM).The incision time was documented to be 15:49 (3:39 PM). Sedation Nurse Beta validated the following vital signs 137/83-101-31-100% 2L. Sedation Nurse Beta documented the cardiac rhythm to be sinus tachycardia and the end-tidal CO2 monitor reading to be 33. Sedation nurse Beta documented the Wisconsin Sedation Scale at 15:57 (3:57 PM) was Moderate (4) Drowsy, eyes open or closed but easily arousable to consciousness with verbal stimuli.
Sedation Nurse Beta documented she administered Fentanyl 25 mcg IV-push at 16:03 (4:03 PM) and Versed 0.5 mg IV-push at 16:04 (4:04 PM). She also validated the following vital signs, 109/66-99-17-97% with etCO2 of 38. Sedation Nurse Beta documents the Wisconsin Sedation Scale at 16:10 (4:10 PM) was Moderate (4) Drowsy, eyes open or closed but easily arousable to consciousness with verbal stimuli.
Sedation Nurse Beta documented she administered Heparin 3000 unit IV-push at 16:13 (4:13 PM). She also validated, the following vital signs, 111/58-98-17-98%, etCO2 37.
At 16:17 (4:17 PM), Sedation Nurse Beta entered a second, “one-click med” for Lopressor 5 mg IV-push.

This medication was not charted as given. Upon information and belief, this medicine was given and started the cascade of events that ensued.
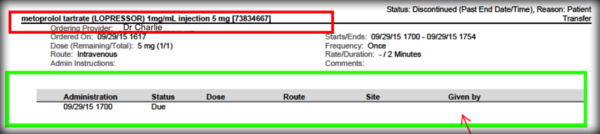
Unlike in the previous “one-click med”, these events were removed from the Audit Trail. At minimum, since it was ordered, and acknowledged, those footprints should have been revealed in the Audit Trail, they were not. In fact, the session number (order number) was not found in these Audit Trails which confirms an active cover-up.
Sedation Nurse Beta validated the following vital signs, 89/52-96-100%. She also documented Heparin 2000 Units given IV push for a total of 5000 units at 16:19 (4:19 PM). Sedation Nurse Beta documented 500 cc of IV fluid was administered. At 16:23-24 (4:23-24 PM), she validated the following vital signs 92/39-81-91% and documented,“suctioned, patient lethargic, Anesthesiologist Dr. Delta called and came in room. Patient given reversal for versed with slight arousal. Anesthesiologist Dr. Delta said he would check back in 5 minutes. Patient continued to deteriorate, (O2) saturation dropping, anesthesia called in STAT again.”
According to testimony from Circulating Nurse Echo, there were some issues with the suction at this time and he left the room to return with a different suction machine.

But Sedation Nurse Beta testified differently.

Sedation Nurse Beta goes on to document, “rapid deterioration of patient vital signs……..code called.”
According to Anesthesiologist Dr. Foxtrot, he testified that he was “summoned to speak with Vascular Surgeon Dr. Charlie in the sedation room”. He testified as below.

According to Anesthesiologist Dr. Golf, he testified he was called to room 20, where he decided to intubate Jane.

What is clear to the Plaintiff is the documentation and the testimony do not comport.
The documentation supports the procedure was finished at 16:45 (4:45 PM). If we believe the general documentation up to this point, Jane was intubated and the thrombectomy procedure was finished. Interestingly, there was a profound void in documentation of Jane’s post-procedures; thrombectomy and intubation which gives pause to the presence of the Sedation Nurse Beta during this time.
It is upon information and belief, that the Defendant has intentionally removed the computer-generated data not only from the chart but also the audit trails provided.
Sedation Nurse Beta began documenting and validating data at 16:55 (4:55 PM).This gap in time coupled with the few medications documented by Sedation Nurse Beta, “1 amp of epi, 1-gram calcium, IV dextrose”,along with verified, oxygen saturation of 60%, give credence to the fact that Jane was in unrecognized PEA (pulseless electrical activity) from 16:45-55 (4:45-55 PM).
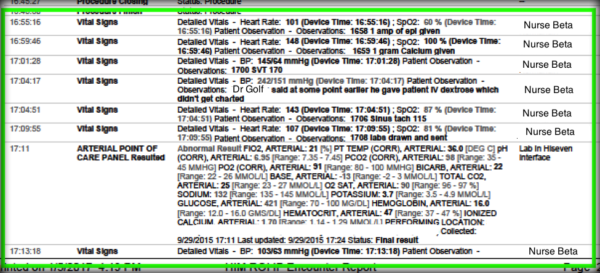

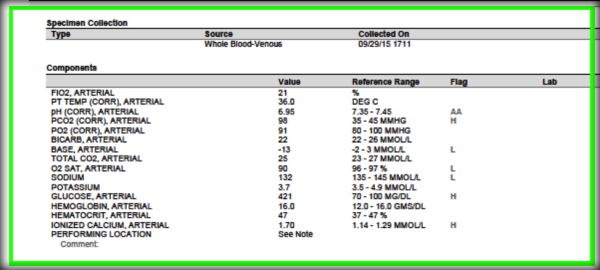
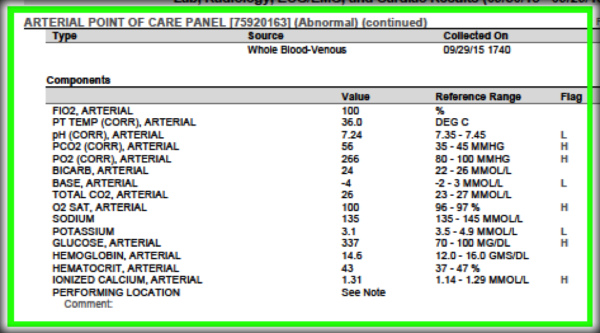
Dr. Golf in his deposition, testified about Jane having an “A-a gradient, which is an index of how poorly the lungs were working usually, and she had a very large A-a gradient, which is – if you’re delivering 100 percent oxygen to some, if they’re very sick, they only get a fraction of that oxygen.”

It is upon information and belief, that one of the possible causes of A-a gradient is ventilation-perfusion (V/Q) mismatch. We believe in this case, Jane was in PEA which means the monitor is reflecting the electrical activity of the heart, but the heart muscle is not responding, and no one recognized this emergent situation. In other words, Jane did not have a pulse hence the ventilation/perfusion. (V/Q) mismatch and profound worsening hypoxemia.
Sedation Nurse Beta validated at 17:01 (5:01 PM), the following vital signs, 145/64 with an “SVT 170”. She also verified continued hypoxia with the oxygen saturations in the 80’s. Sedation Nurse Beta, documented labs were drawn at 17:08 (5:08 PM). The arterial blood gas (ABG) was resulted at 17:11 (5:11 PM). This ABG reflects a profound acidosis with a pH of 6.95 and a pCO2 of 98. This clearly supports the ventilation/perfusion (V/Q) mismatch.
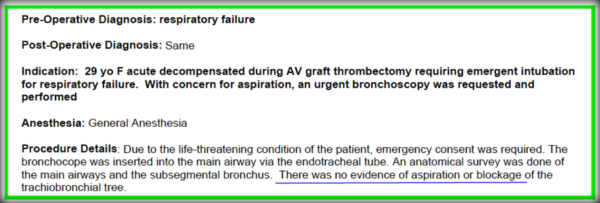
According to testimony, Pulmonologist Dr. Hotel was called for urgent bronchoscopy. Sedation Nurse Beta documented the bronchoscopy was performed at 17:20 (5:20 PM). The findings are below.
An ABG was resulted at 17:40 (5:40 PM), which confirmed the ventilation/perfusion (V/Q) mismatch was NOT related to her lung compliance. Her oxygen saturation on 100% FiO2 was 100%.
According to documentation, Jane arrived in the ICU at ~ 17:58 (5:58 PM). She was ultimately diagnosed with a profound hypoxic ischemic brain injury. Jane had a long-convoluted hospitalization. She suffered from seizures, required a tracheostomy, PEG tube and was completely dependent on staff for her all of her ADLs. Jane suffered numerous hospital-acquired infections, and decubiti. Ultimately, she suffered refractory shock from sepsis and died July 22, 2016.
The following list includes, but is not limited to, deviations in the standard of care:
- Evidence of failure to recognize and fully treat the crisis of hypoxemia (decreased oxygen) and hypoventilation (increased CO2).
- Evidence of failure to fully reverse the sedation which caused hypoventilation.
- Evidence of unqualified staff performing sedation.
- Evidence of chart manipulation (deletions, and/or intentional omissions).
- Evidence of failure to concurrently document the medical interventions which occurred. This is a violation of standard policies and procedures of hospitals.
- Evidence of unqualified staff performing sedation.
- The medical records severely misrepresent what occurred in this case and the evidence confirms a systemic cover up from the top of the corporation down to the clinical staff.
This was ultimately an indefensible case for the Defendant. This case settled for a confidential amount.
In-depth case review is about more than simply providing a summary of events that are documented in the medical record. The professionals at ADROITSM view each medical case with a forensic and legal lens. The veracity of testimony, discovery, and medical records are tested against years of experience to insure the legal team operates with the best information. ADROIT® stands ready as a resource for your team. Give us a call.
