This blog is about how two particular industries must adapt to provide services for an increasingly diverse population. An orientation and gender diverse population is emerging from the shadows seeking acceptance, understanding and equality.
The ever-increasing separation from age old social constructs presents a challenge across all service industries. Hospitals and medical providers are challenged by these questions because an understanding of biological gender is important to understanding disease process, diagnostic lab value norms, predisposition to known illnesses and reproductive status. Hospitals and medical providers also have to make every effort to provide for the psychological well-being of their patients and protect their privacy. The forward push toward changes in care delivery goes beyond a simple enlightened understanding of gender, it’s a matter of financial viability as well.
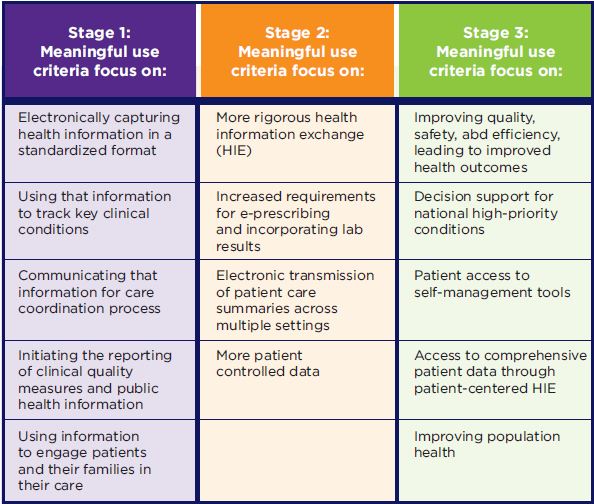
In October of 2015, CMS, the Centers for Medicare and Medicaid Services, announced the requirement for the collection of SOGI (Sexual Orientation and Gender Identity) data by health care providers, and the incorporation of such data into the EHR (electronic health record) as part of the Meaningful Use Incentive Program. This move was supported by the Joint Commission and the IOM (Institute of Medicine), (Sean R. Cahill, 2016). The Meaningful Use Incentive Program is an initiative of CMS that rewards medical care providers with a financial incentive for the adoption of “meaningful use” of EHR (electronic health records) for improved quality, safety and efficiency of patient care. Meaningful use was set to be rolled out in stages with the intent of improving health outcomes, reducing health care cost and eliminating health disparities, (see figure 1 below). For this and other reasons, hospital systems and medical care providers are adapting electronic medical record (EMR) systems to better identify patients that have a different gender identity than the gender assigned at birth. This process is still in its infancy and looks different in various hospital systems but essentially is designed to do the same thing; enable providers to diagnose and treat illness and injury in patients based upon their gender at birth while facilitating productive patient care relations in consideration of their gender identity.
This issue is highly complicated. Let’s use a theoretical case example to illustrate some of the challenges. A 24-year-old patient reports to the emergency department with a complaint of abdominal pain. A case like this will trigger a number of diagnostic tests to include a urinalysis, a complete blood count (CBC) and a complete metabolic panel (CBC). If this patient’s gender at birth is female, a urine pregnancy test will also be ordered. This is not only to determine if the abdominal pain is associated with a possible pregnancy but also to determine if precautions need to be implemented for diagnostic scans. How this patient is listed in the EMR will determine reimbursement status from medical insurance. If this patient was identified as a male, the insurance company would not reimburse for a urine pregnancy test. If the patient’s gender at birth was female, yet the patients gender identity was male, the urine pregnancy test would still need to be performed but the patient has to be coded in such a way as to facilitate payment by the insurance company. This is just a simple example of the challenges associated with diagnosis, treatment and billing for a patient who’s gender at birth does not match the gender identity. In spite of the best efforts to prevent errors, complexities of this nature are likely to result in misdiagnosis or mistreatment.
Identification of the patient is another challenge. Hospital red rules dictate that patients are identified before the administration of diagnostic testing, blood collection and medication administration. This is typically done through the use of a patient armband with patient identifiers. A disparity between proper identification of a patient and respect for patient preferences can arise under certain circumstances. If a patient’s gender at birth and gender identity do not match, and the patient has adopted a name more appropriate to the gender identity without legally changing the name, a disparity results between the patients preferred reference and the legal reference for the patient. This poses another challenge to medical staff that is required to use patient identifiers to verify a patient before enacting diagnostics or treatment. If a disparity exists between the legal gender determination and the patients gender identity, this can also pose a challenge.
These issues create challenges and opportunities for the legal profession, just as it does with the medical profession. Future forward law firms can preemptively adapt their practice and be aware of these issues, thus benefitting from the opportunities without struggling with the same challenges that are faced by most businesses. What specific opportunities and challenges does this issue present to today’s law firms? Let’s start with the opportunities.
As health care providers struggle with the issue of gender identity, Murphy’s law will dictate that some things are not handled correctly. There is ample opportunity for health care providers to misdiagnose or mistreat patients because of a misunderstanding of their birth gender/gender identity. When, and I say when and not if, these things occur, the patient or patient’s family will be seeking future forward law firms that understand these issues to take up their cause and represent them to pursue damages. Law firms that are behind the times, have a greater chance of fumbling the game ball in these situations. There is also ample opportunity for individuals that have suffered discrimination as a result of their gender identity to pursue damages from a myriad number of sources including health care systems that have not adjusted to the reality of the emerging understanding of gender identity. The opportunities abound from there, but the challenges posed swing the pendulum into balance. The challenges posed will be addressed in our next blog as the social aspects are discussed.
The consideration of the medical implications for a gender diverse population in medical malpractice, though complicated, can still be navigated successfully with a comprehensive approach. ADROIT®is an experienced resource to aid legal teams in the pursuit of justice even in these uncharted waters by giving a Medical Analysis with a Legal Perspective.
The next article will address the social aspect of gender diversity and its impact on legal cases and juries.
- Garnett, B. (2019). Print Version PDF Print Logo Clinical Care Extenders Play Critical Role in Meeting Meaningful Use. Retrieved from Cope Health Solutions: https://copehealthsolutions.com/cblog/clinical-care-extenders-play-critical-role-in-meeting-meaningful-use/
- Sean R. Cahill, P. K. (2016). Inclusion of Sexual Orientation and Gender Identity in Stage 3 Meaningful Use Guidelines: A Huge Step Forward for LGBT Health. LGBT HEALTH, 3(2), 100-102.
